The deadline to adopt ICD-10 has officially passed, and the transition has had a major impact across your organization as everyone learns and adjusts to the new codes. So what's next? As you continue to see just how big ICD-10's impact is, now is a great opportunity to be proactive about any complications and inefficiencies it has caused.
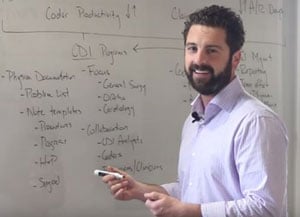
Director of Optimization Rick Shepardson discusses the range of issues from physician documentation to more A/R days that you may have begun to encounter as a result of ICD-10. In this video, he'll show you how Nordic can help you decrease denials and improve your revenue cycle.
Watch the video to see what else to expect.
Time: 11 minutes, 11 seconds
Transcript
Rick: Hello. Today we're here to talk about ICD-10. Now, it's after October 1, so you probably know a lot about ICD-10. You probably already had to go through it. You've probably done a lot of work to get everyone on your team educated. You probably also did a lot of work to make sure that you worked with payers and to make sure that you knew whether or not they were going to support ICD-10, if there were any changes to your expected reimbursement contracts, etc. Probably also did a lot of work with dual coding, making sure that you understood the impacts of ICD-9 to ICD-10 and where your organization may struggle. That really helped to get the coders and the physicians moving in that direction. That naturally led to testing. You probably worked with your payers. You probably also worked on testing your EHR. Is that ready to go? As we got closer to the date, there was obviously the step of conversion, so making sure that the new code sets are in place, and making sure that preference lists are updated.
Now, you got to October 1, and you're ready to go. Well, October 1 is really just the beginning. As you move forward, we're going to have claims out the door. As those claims get paid, we move on. We get payer responses. As those payers respond, well, you may get denials. You may not get reimbursed as much as you're thinking. This is really going to happen in perpetuity. People are going to be working on ICD-10 up till we get ICD-11. I know everyone's excited for that. Well, along the way there's a lot of potential problems we're going to run into.
Physician documentation is more important than ever. It's important that they are documenting with the right specificity, making sure that the documentation is going to support the diagnosis or the procedure that needs to be coded. We're also going to look at coder productivity. Coder productivity is predicted to plummet, go way down, 20 to 40% decreases. It's going to be a lot harder for coders to find all of the documentation needed to support their coder diagnosis. They're also learning ICD-10 as well, obviously. As they become more and more proficient, the productivity will start to go up but at least up front, we'll see significant hits. Because the documentation and the coding processes are not quite fluid yet, we're going to expect claim errors to increase. If the claims aren't right, well, they're probably going to get denied, at least sometimes, so denials are expected to increase significantly.
 What is all of this what's this going to lead to? These are really going to lead to an increase in A/R days. You're trying to get this money in. Hopefully, you've been able to build up a nice cushion of cash to weather that storm, but there are going to be concerns there. As the productivity goes down, and there's more back and forth with the physicians, well, this is also going to lead to an increase in discharged not final billed, which relates back to A/R days but with slightly different metrics of where we're expecting to see impact. Well, as all of these things are impacted, it's important that we, the organizations, have a plan how to address them. How do you make sure that you can get back to status quo as soon as possible?
What is all of this what's this going to lead to? These are really going to lead to an increase in A/R days. You're trying to get this money in. Hopefully, you've been able to build up a nice cushion of cash to weather that storm, but there are going to be concerns there. As the productivity goes down, and there's more back and forth with the physicians, well, this is also going to lead to an increase in discharged not final billed, which relates back to A/R days but with slightly different metrics of where we're expecting to see impact. Well, as all of these things are impacted, it's important that we, the organizations, have a plan how to address them. How do you make sure that you can get back to status quo as soon as possible?
Here at Nordic, we really think that there's a two-pronged approach to making this happen. We focus on denial management and clinical documentation improvement programs. As we look at denial management, really what a lot of this is about is about reporting, making sure that you're getting as much detail back from the payer as possible so that you understand why your claim got denied, and also having more of a team effort to work on these denials. What's the role of physicians? What's role of case managers? Who knows everyone that you want to get involved? Having a plan for how to stratify those denials that come in and then making sure that the right people are involved in addressing them, is going to be critical to success just as it is today. It's just a new focus.
Within the CDI program, as you're going with your dual coding, and as you understood some of the research, you probably understand the key areas to focus on. Making sure that focus is built into your EHR or your CDI program is the next step, making sure that is very transparent and clear. From what we understand from research that has been completed, the key focus areas are going to be those high-dollar, high-volume areas. General surgery is going to be hit hard, ortho, cardiology. As we move forward, making sure that these areas are a part of your physician documentation improvement efforts will really ensure that it's a team effort. You're improving documentation as you're identifying ways to improve your coding.
The other part of the CDI program is really important for collaboration again. There's a lot of groups that need to be involved. Obviously, you'll have CDI analysts, who can be working through reviewing the documentation, making sure that it is going to be sufficient to support coding. You also have an opportunity to work with those coders to make sure that they're involved and that they're ready for that hand off. As soon as the patients been discharged, we hit min days, and we're ready to go, ready to hit coding. So that should start to improve your coder productivity. Also physicians or clinicians in general, making sure that they're involved and they know what they're role is. They can help improve the documentation as needed in the query process back and forth. Making sure that this process is managed is going to be critical to making sure that those bills get out the door in a timely manner.
As this starts to focus in and you start to really collaborate and making sure that everyone is taking part in these efforts, actually improving the physician documentation is going to critical. Obviously, there's a few places that you're going to want to focus. Making sure that the problem list is being used appropriately, is comprehensively got all the problems on there, maybe you have problem oriented charting. You also want to be working on note templates and documentation templates. These templates can be used for everything from procedures to progress notes, to H&P notes, to surgical notes. Really making sure that the physician documentation is templated and discrete is going to increase the likelihood that it's going to be specific enough to meet documentation needs, meet coding needs.
As we finally involve coding in this process, really making sure that they're checking for medical necessity, and as they are collaborating with the CDI analysts, they really should be able to focus on only clarifying those nuances, really making sure that the codes are more accurate. As we get better and better accuracy of coding, well, that should start to mean that the claim errors are going to decrease. As the claim errors decrease, the denials should start to decrease. You're still going to want this feedback loop where the denials and the denial reporting is informing the CDI program in terms of what they should be focused on, but it's going to be a more holistic process.
So we're tying together functionality and work flows, operational processes, and accountability for denial management. We're using that to inform your CDI program, making sure that they're focused in the right areas and working across all of the team members, to then ultimately focus on improving clinician and physician documentation. We're doing this all while keeping everyone educated in terms of what's the latest? What's happening in our organization? What does all this documentation and work mean? What does this mean to the bottom line? That is going to really allow your organization to come together cohesively, be able to meet these challenges head first, and make sure that your AR days start to creep back down again.
That's all I have for you today. Hopefully I'm going to get to talk to you again in the future. Hopefully you're going to be successful with ICD-10. Thank you for your time.