 There is a lot of hype today about healthcare interoperability and the promise of standards-based healthcare data exchange. I’m a big believer in it myself. I see some interoperability technologies that are currently emerging and maturing as the crucial next step towards true innovation in healthcare. But what makes the latest technology and standards any different?
There is a lot of hype today about healthcare interoperability and the promise of standards-based healthcare data exchange. I’m a big believer in it myself. I see some interoperability technologies that are currently emerging and maturing as the crucial next step towards true innovation in healthcare. But what makes the latest technology and standards any different?
Technically we’re just taking another step in a long journey. This is the same journey that we were on in 2009 when the HITECH Act created the Meaningful Use program and electronic health record (EHR) adoption skyrocketed. This is also the same journey we were on when HL7 V2 messaging was introduced 20 years before that.
Is it really fair to our history, and to all the sweat and tears behind us, to say that we’ve finally arrived at that holy grail of interoperability? Not by a long shot. There is still far more work to be done. We are many steps closer than we were a decade ago though, and we have built and deployed the technical groundwork that will serve us for decades to come.
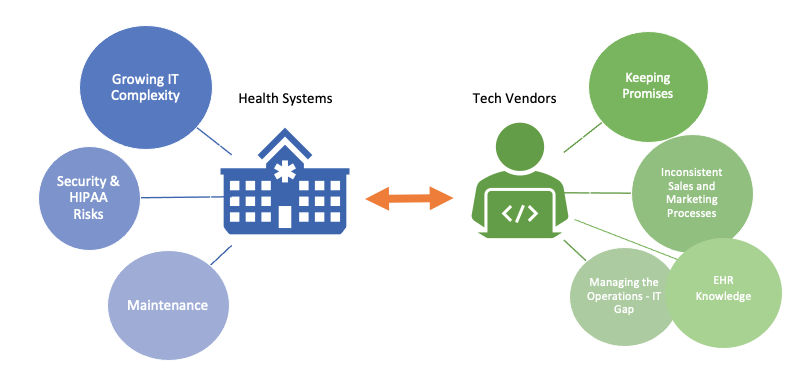
This change has come about slowly, however. Technology adoption by health systems is still sluggish; the sales cycle can range from anywhere between eight and 18 months. It’s easy to see why, as large bureaucracies, complex security concerns, and intricate IT ecosystems create barrier after barrier. But what’s still stopping us from breaking down these barriers?
Here are a few insights we’ve uncovered over the years:
Health system value vs. effort
Healthcare systems and their employees often view interoperable technologies not based on the benefits they provide, but on the challenges they pose. Most technologies don’t directly benefit the people and groups who implement and maintain them, which creates a separation between the derived value of the technology and the efforts to support it. Application implementers at the health system inherently seek to limit the number of applications adopted because of the work effort associated with each implementation. This makes it more difficult and expensive to launch an application and gain traction in the marketplace, which stifles innovation.
Health systems and application vendors can overcome this through additional technical and practical advances. As EHRs and integration standards mature, the burden of application implementation drops. Today, application vendors and health systems should cooperate to share implementation knowledge and lessons learned. Each application implementation should result in improved project plans and build trackers, new build import tools, and checklists or other “deep dive” materials for complex setup steps.
The operations – IT gap
Because of the value vs. effort divide discussed above, an application vendor’s approach to health system relationships should be two-fold: sales and support of the application from the operational or user standpoint and the same from the IT standpoint. Application vendors should approach and plan for these concepts separately. We encourage operations to involve IT early in the sales process and vice versa, as well as bring unique collateral to different discussions with each unique group.
EHR secrecy
Finding information on EHR integration can be very challenging. Understanding it, even more so. We often see health systems and application vendors work together to share integration information, desired future state concepts, and more. When in doubt, make sure you understand the standard you’re using to interoperate and build a shared vocabulary with your clients. Strong communication principles will foster success.
I also encourage screenshots wherever possible. The Patient Access and Interoperability rule, a result of the 21st Century Cures act, requires that EHR vendors strip clauses from their contracts banning the sharing of EHR screenshots and workflow videos. In many cases, it is now OK to display screenshots of in-EHR workflows for sales and implementation purposes.
Implementing an application within an application
Interoperable applications are integrated by definition, and that integration is most commonly with the EHR. The vast majority of applications Nordic works with integrate some front-end functionalities directly into the EHR or patient portal. Your application is now a feature or module within a broader application. This change in approach impacts design and UI of the application, authentication, data transmission protocols and data structure, navigation between pages and functionalities, browser and version support, and much more.
Application vendors should support standards-based methods wherever possible to ease application integration and work with users to understand how the application fits into the broader context of their workflows. Your initial implementation should be a testing ground; prepare for UI and integration changes as a result.
Security and HIPAA
No matter how well built an app is, it is always a security risk. Due diligence takes time and costs money. Health systems must balance security risks with the demand for new and better tools, drive to innovate, and more. App vendors should be prepared to speak in-depth during the sales process about how their applications are designed to mitigate risks and protect data, how the applications are tested to identify vulnerabilities, and how their companies will respond when a security incident takes place.
Numerous security risk certifications and assessment standards exist today. These concepts help both parties communicate a set of standards rapidly. I recommend app vendors pursue an appropriate security certification primarily because stating “Our application is CSA STAR Level 1” is much simpler than communicating that you meet each of the 300+ requirements included.
A jack of all trades
Any application, no matter the scope, is just one piece of a large technology puzzle, and IT personnel must have a hand in it all. FHIR APIs and HL7 interfaces are certainly important, but they aren’t the only thing to worry about. Ground-level analysts who oversee the technologies an app utilizes likely oversee tens of other apps and systems. Application vendors should be sensitive to this constant pull from all directions. This is why so much of my advice centers on simplifying the sales, communication, and implementation processes for an application.
Nordic is well positioned to help break down these barriers. At our core, we are EHR experts, with over 1000 employees working at health systems across the U.S. and internationally. Our Interoperability team spends our days building FHIR and SMART on FHIR functionalities for application vendors as well as implementing and managing our own application with health systems. We have the privilege of learning from many smart people in the industry and assisting them as they tackle EHR integration challenges. This breadth of experience, from our roots to our daily interactions, gives us a unique insight into the world of healthcare interoperability. We get to see successes and learn from the challenges facing a broad array of stakeholders.
Want to learn more about how Nordic can help you break down interoperability barriers?
