At its heart, health IT is about improving the lives of patients and their families. When an EHR works well, it makes information more accessible, mistakes less frequent, and healthy living easier. As a healthcare consulting firm, we know health IT can transform care and drive better outcomes.
But when budgets and user dissatisfaction are clamoring for attention, patient impact isn’t always the first thing on our minds. When stress levels are high, it can be hard to remember that our work – the meetings, the hours of build, the late nights on go-live – is paying off to improve patient care.
That’s why we'd like to give you a chance to reflect on a project that embodies the impact of EHRs on patient lives. After all, we believe that health IT – and the experience we’re about to share – is worth celebrating.
The challenge
Last year, Nordic had the privilege of working with The University of Maryland Medical System (UMMS) to answer a common question: How do you use your EHR to improve population health without creating more work for providers?
At UMMS, the focus of this question was HIV and Hepatitis C virus screening and linkage to care.
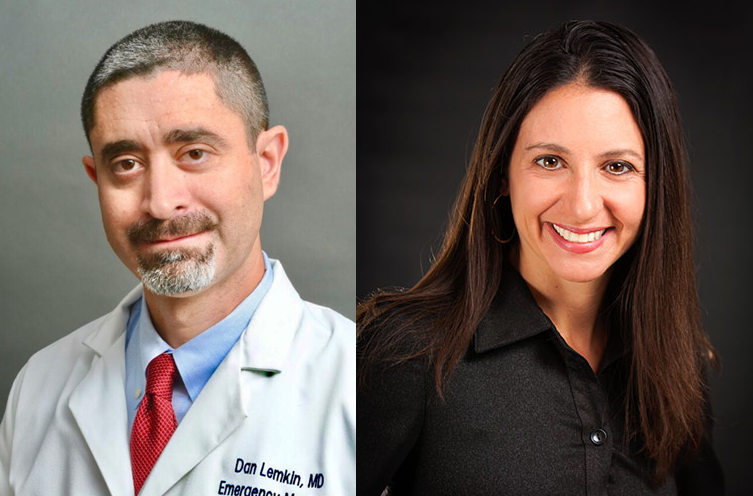
Dr. Dan Lemkin, University of Maryland Medical System; Jamie Mignano, JACQUES Initiative
UMMS wanted to increase the effectiveness of HIV and HCV screenings in the inpatient, ED, and ambulatory settings, while minimizing impact on providers. The ED was a common target for EHR initiatives, and leadership knew that compliance would be challenging if another project were introduced.
“HIV and HCV screenings are crucial to patients’ health,” said Dr. Dan Lemkin, UMMS director of clinical informatics. “From improving outcomes to reducing utilization, there are many good reasons to do a project like this. But the operational reality is there is a lot of scope creep here. You’re asking providers to take time out to engage a specific issue.”
To address this challenge, The JACQUES Initiative of the Institute of Human Virology at the University of Maryland School of Medicine – a program aimed at improving access and engagement in HIV/HCV care – created the idea to build EHR functionality to automate patient identification and provider notification.
By automating these processes, the team believed they could increase screening rates without increasing workload, helping to improve the health of a vulnerable population.
The process
To automate HIV/HCV screening processes, The JACQUES Initiative’s Executive Director Jamie Mignano submitted a grant to fund the project and partnered with Dr. Lemkin’s team. They engaged two Nordic senior consultants, myself and Michael Stineman.
To get providers on board, Dr. Lemkin laid out some expectations. He wouldn’t ask providers to complete additional data review for every patient who came through the door; instead, the EHR would automate testing identification, and providers would only review data for intervention.
Now came the challenging part: Building out rules that the EHR would use to identify patient needs and tie those needs to recommended actions.
For example, patient needs differed depending on past HIV and HCV status, age, location, and other factors. To make sure patients were treated correctly, the team built a scoring system within the EHR, which channeled patients to different outcomes based on characteristics.
“One situation we were interested in was a patient who had received an HIV test that had returned positive,” Dr. Lemkin said. “In our matrix, that resulted in a score that sent a silent In Basket notification to prompt follow-up to The JACQUES Initiative team of linkage to care navigators.”
The team started by building the functionality in UMMS’ ED and inpatient departments, then in the University’s Midtown campus and ambulatory clinics.
Nordic Senior Consultants Michael Stineman and Katy Ptaszynski
The results
The build introduced several functionalities to UMMS’ EHR. The optimized system is now able to identify patients based on screening need, automate orders for patients who meet criteria, recommend follow-ups to providers, and offer an at-a-glance view of patient status.
The system also enables a variety of staff, including nurses and medical assistants, to address the Best Practice Advisories, which helps manage provider workload and ensure follow-ups. And the system alerts the care team of previous positives, since more than half of people living with HIV and HCV aren’t in care.
The system also helps with follow-ups and prevention by using rule-based logic to incorporate patient education and resource information into the After Visit Summary, depending on testing results.
The optimization has been innocuous for providers.
“We didn’t get any complaints from providers, because the alerts weren’t intrusive,” Dr. Lemkin said.
When it comes to patient care, the results have been staggering.
“We’ve successfully recorded 100 new HIV diagnoses at our two hospitals,” Jamie said, “and about 80 percent of those folks have followed up with getting care. For HCV, almost 20 percent of the 7,000 persons screened have a positive antibody test and required further testing and linkage to care.”
Dr. Lemkin and Jamie say the work has been critical to improving intervention for HIV/HCV patients and funneling patients from the acute care center into an ambulatory setting. When HIV/HCV patients can be quickly identified, triaged, and reached for a follow-up, they’re more likely to receive the care they need.
“These automated programs, where we can leverage technology to mitigate the impact on providers while improving population health, are crucial,” said Dr. Lemkin.