 Back in the bad old times of medicine (defined by many of us as “before I was practicing medicine”), most physicians were easy to spot. They wore long white coats, had a stethoscope hanging around their neck, and carried a prescription pad in their pocket. Oh, and in the United States, they were virtually all White men. That last fact is important. Since the average American typically lacks the specific medical knowledge required to make important life decisions, we often ask our doctors: What would you do if you were me? The answer may be right for the physician, but it is often not right for the patient.
Back in the bad old times of medicine (defined by many of us as “before I was practicing medicine”), most physicians were easy to spot. They wore long white coats, had a stethoscope hanging around their neck, and carried a prescription pad in their pocket. Oh, and in the United States, they were virtually all White men. That last fact is important. Since the average American typically lacks the specific medical knowledge required to make important life decisions, we often ask our doctors: What would you do if you were me? The answer may be right for the physician, but it is often not right for the patient.
With regard to the homogeneity of American doctors, the times, they are a changin’. According to a recent report by the Association of American Medical Colleges, as of 2021, some 37% of active physicians in the United States were women, and 47% of residents and fellows were women. This is a landmark improvement, but as William Gibson said about the future, it’s “already here – it’s just not evenly distributed.” As of the latest data, women accounted for 65% of active physicians in pediatrics, but only 6% of active orthopedic surgeons. This represents uneven distribution, indeed.
On the race and ethnicity side, the data show similar improvements, but also significant room for improvement. About 64% of practicing physicians in the U.S. were White, while about 20% were Asian, 7% were Hispanic (regardless of race), and about 6% were Black. Given that roughly 13.6% of Americans are Black, the gulf between where we are and where we need to be is wide.
These statistics matter because so many important decisions that patients must make about their health involve nuanced questions with incomplete and/or rapidly changing evidence. While physicians naturally want to help their patients choose the best options, they often make recommendations based on what they would do, assuming that their socioeconomic status, values, goals, and ideals are in line with their patient’s. Even with the best intentions, unintended biases due to race, ethnicity, gender, etc., can occur, altering the course of care.
To equip patients to make the best choices, we leverage shared decision-making, defined as “a process in which clinicians and patients work together to make decisions and select tests, treatments, and care plans based on clinical evidence that balances risks and expected outcomes with patient preferences and values.” While this seems straightforward and obvious, the real-world application is more arduous.
A recent viewpoint article in JAMA Cardiology outlines some of the issues of shared decision-making with respect to aortic stenosis (AS). Megan Coylewright, MD, MPH, a cardiologist at Erlanger Health, notes that there are many exciting new treatment options for AS, yet it can be difficult to know exactly how to get to the “right” answer for a given patient. She writes, “Literature abounds on ‘lifetime management’ of AS: valve performance across valve types, procedural risk, durability, and coronary access. Global meetings feature presentations on techniques for valve explant; modeling of valve in valve using advanced imaging; and strategies to split aortic valve leaflets, to name a few of the technical ‘hot topics.’”
“In contrast,” she continues, “there is comparatively limited attention paid to which treatment features patients value most and strategies to address them. Discussion of how to communicate choices while engendering trust, exploring goals, and minimizing fear of future risks are rare.” It’s easy to talk about the technical aspects of care (e.g., how we use advanced imaging to best model the aortic valve), but more difficult to comment on the “soft” aspects of care (e.g., actual quality of life after a complicated intervention).
What’s a physician to do? A key aspect of shared decision-making involves patient decision aids, adding a more objective or illustrative aspect to the difficult conversation. Based on specific data points of the patient, a personalized risk profile can be generated. Yet, we know that from a human-centered design perspective, percentages and dry calculations can be difficult to truly internalize. Incorporating graphics into the mix can make all the difference. For example, it’s one thing to know that a potential intervention (in this case, taking anticoagulation medication) will decrease the risk of stroke by almost half (from 12% to 7%), yet another thing to see a graphical representation. Here’s one example from the literature:
Figure 1
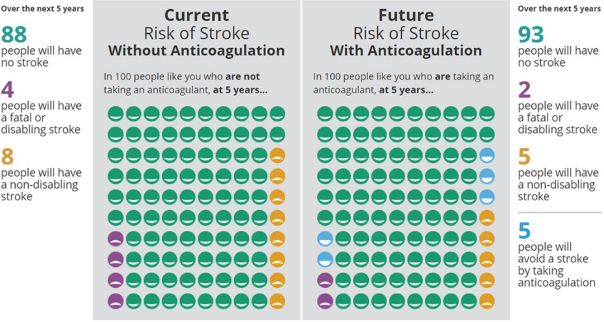
Note. From Noseworthy PA, Brito JP, Kunneman M, et al. Shared decision-making in atrial fibrillation: navigating complex issues in partnership with the patient. Journal of Interventional Cardiac Electrophysiology : an International Journal of Arrhythmias and Pacing. 2019 Nov;56(2):159-163. DOI: 10.1007/s10840-018-0465-5. PMID: 30327992; PMCID: PMC7056296.
It’s easier for a patient to make the appropriate decision if they’re able to process the data points in a more relatable way.
So how do we continue to use shared decision-making as the standard of care? We must acknowledge that the background of a particular physician or other care team member will affect how they make recommendations and what those recommendations are. We need to keep developing shared decision-making methodologies and incorporate them into undergraduate, graduate, and continuing medical education. Finally, we should insist that patient decision aids evolve and are incorporated into electronic health records and patient portals so they can be used at the point of care, when life-and-death choices are being made.